You probably know Alzheimer’s gets a lot of the spotlight when we talk “dementia.” But talk to any neurologist or neuropsychologist, and they’ll tell you: vascular factors lurk behind way more cognitive decline than we admit.
And now, thanks to a new international consensus, the game is changing. Meet VasCog-2-WSO, the updated diagnostic criteria for vascular cognitive impairment and dementia (VCID). They’re not just a tweak—they’re an attempt to standardize how clinicians and researchers everywhere talk about “brain + blood” damage.
What’s Even Changing?
In 2025, more than 50 international experts used a Delphi-method survey to agree on new criteria for VCID—covering preclinical, mild, and major impairment stages.
Big changes compared to the 2014 VasCog version:
- Operationalized thresholds: Now the criteria give more concrete cutoffs (not just vague descriptions).
- Biomarkers & imaging, not as mandatory stars, but as optional beacons that can flag other or coexisting pathology.
- Preclinical / at-risk category: You can now be flagged before severe symptoms emerge, which opens doors for earlier intervention.
- Official endorsement by World Stroke Organization (WSO) gives it international teeth.
So essentially: more clarity, more flexibility, more room to catch problems early.
Why This Matters
Before this, diagnosing vascular cognitive impairment was messy. Different hospitals and researchers used different standards—some based mostly on imaging, others on how severe the symptoms were. That made it hard to compare studies or ensure consistency in care.
With VasCog-2-WSO, the hope is that a patient in Tokyo, Austin, or Nairobi gets assessed with the same language. The same benchmarks. The same “this is mild, this is major” definitions. That helps us compare studies, track progress, and (ideally) test therapies in a more reliable way.
Key Pieces of the Criteria
Let me break down the big features:
| Feature | What’s New/Emphasized | Why It Helps |
| Pre-clinical/At-risk VCID | A stage before overt symptoms | More window for prevention/intervention |
| Operational thresholds | Concrete cutoffs (e.g., cognitive tests, imaging) | Less ambiguity = better consistency |
| Biomarkers & imaging as flags | Not required, but useful for “is there something else going on?” | Helps distinguish mixed disease (vascular + Alzheimer’s ect.) |
| Stage categories | Pre-clinical -> Mild -> Major VCID | Clearer steps in progression, more clinical “bins” for study |
Challenges & Questions Still in the Room
No update is perfect (and you know I love the messy middle). Here are a few things I’m watching:
- Access & equity: Biomarkers and advanced imaging are expensive. In low-resource settings, the new criteria might be harder to implement.
- Overlap with neurodegeneration: Many people have mixed pathology (vascular + Alzheimer). The criteria allow biomarkers to suggest other causes, but it’s still tricky disentangling.
- Thresholds vs individual variance: Brains aren’t one-size-fits-all. Some people have lots of vascular “hits” but functionally compensate well (cognitive reserve).
- What “preclinical” really means: How far do we push “at-risk” before we risk over-diagnosis or unnecessary anxiety?
How It Connects to What We Already Know
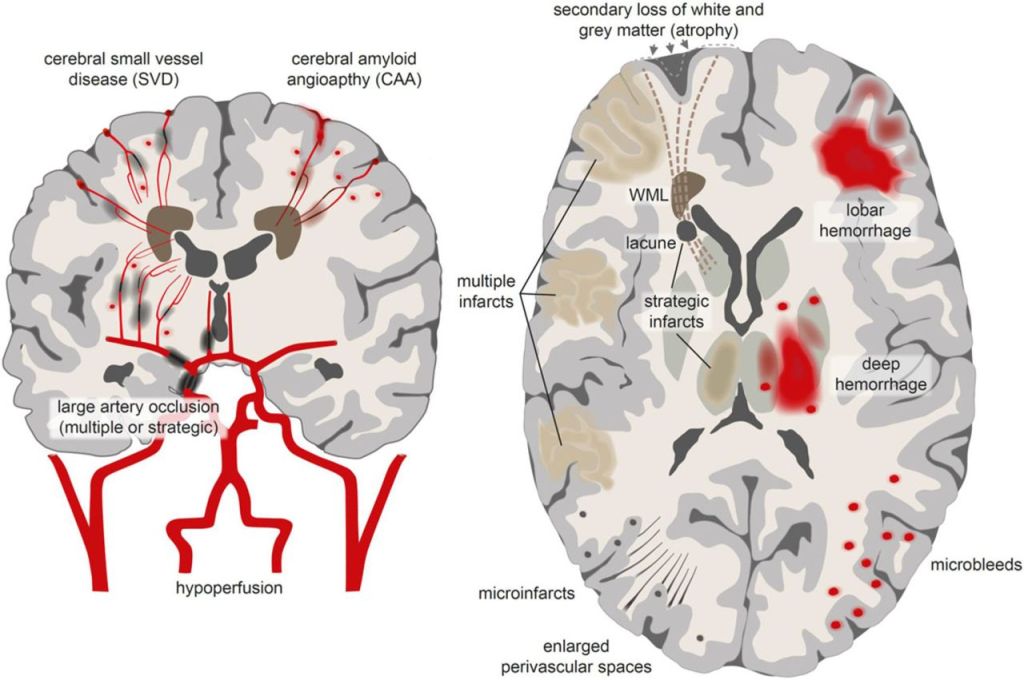
This update is building on decades of vascular cognitive impairment (VCI) research. The concept has evolved from “vascular dementia” (big strokes = cognitive decline) to a spectrum, including small vessel disease, white matter lesions, microinfarcts, and how these affect connectivity in neural networks.
Interestingly, in VCI, processing speed and executive function often take the hit before memory does—a contrast with classic Alzheimer’s patterns.
So the new criteria lean into that: cognitive tests used should match the vascular pattern (not assume the Alzheimer memory-first route).
Why You Should Care (Yes, Even You)
This feels abstract, but it has real impact.
- Better diagnosis: Someone struggling with “brain fog” + vascular risk (hypertension, diabetes) might now be flagged earlier using these criteria.
- Better trials: Standardized criteria mean drugs or lifestyle interventions can be tested in comparable groups everywhere.
- Prevention & awareness: Having a preclinical VCID stage changes the conversation from “treating decline” to “protect your brain now.”
- Bridging specialties: Neurology, stroke, geriatric medicine, neuropsychology—all gain a common language to talk VCID.
In True Mind & Medicine Spirit
Imagine a brain like a city with roads (blood vessels) and neighborhoods (neural circuits). Over time, those roads get potholes, detours, blockages—and parts of the city slowly lose connectivity. You might notice hesitation, slower decisions, weird small mistakes. But you’re still functioning.
VasCog-2-WSO is like giving the city a new, more sensitive traffic-reporting system. Instead of waiting for whole neighborhoods to black out (“dementia stage”), you get early warnings—maybe a side street clogged, a bridge losing maintenance. Then you can fix before complete shutdown.
It’s not perfect—but it’s a meaningful rewrite of how clinicians and researchers will talk about vascular damage to the brain.







Leave a comment